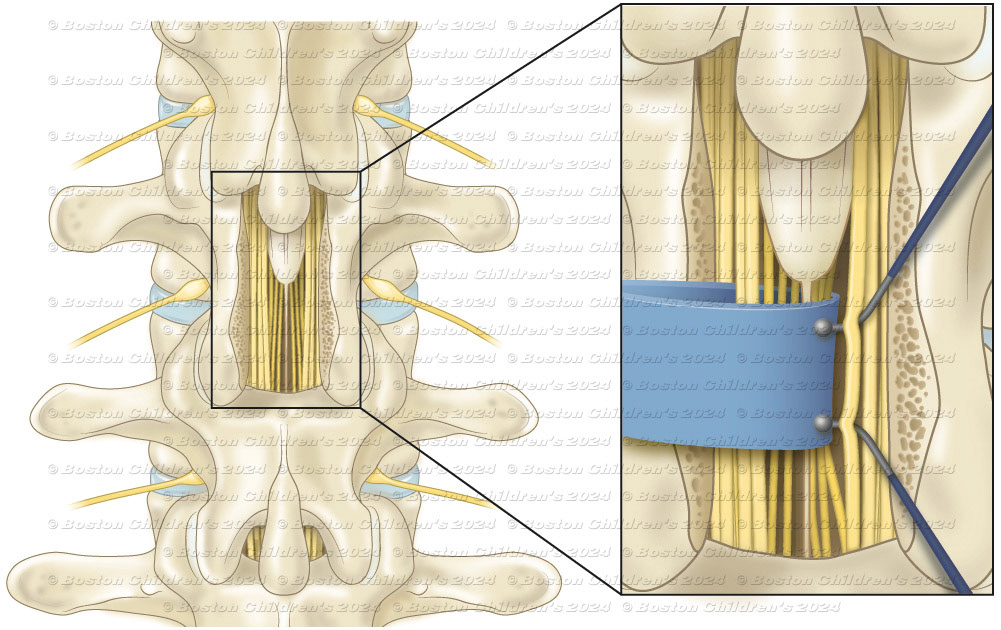
Combined Rhizotomy: a small window of bone removed in order to see the spinal nerves.

The nerves are each tested with small electrical probes. A small rootlet is isolated and cut.

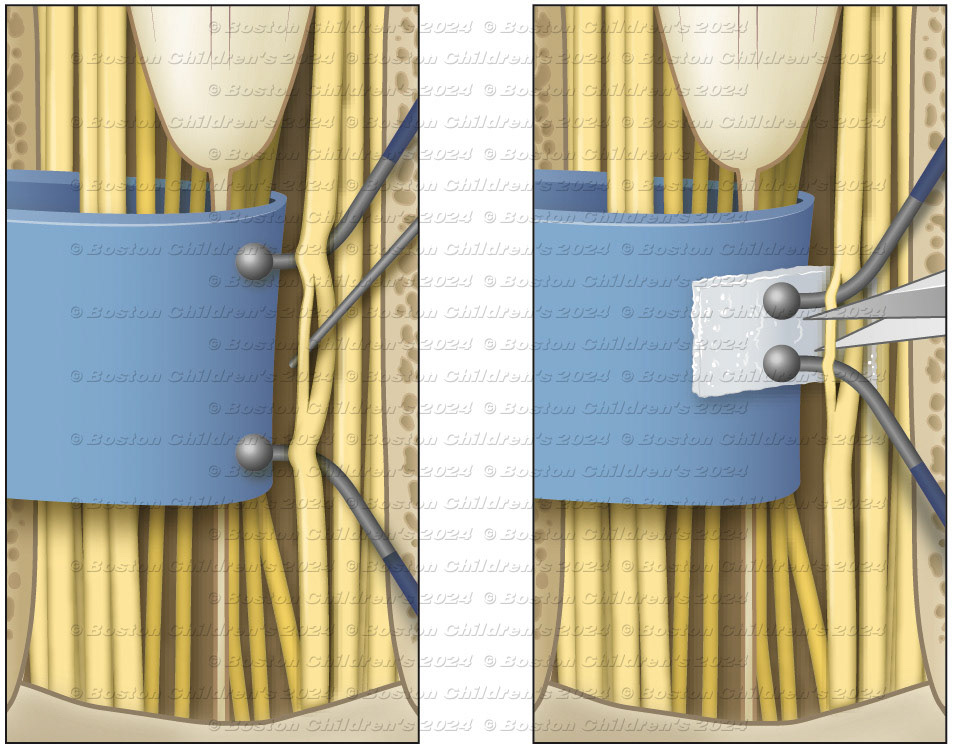
Lumbar vertebra

Applied Cognition, glymphatic system

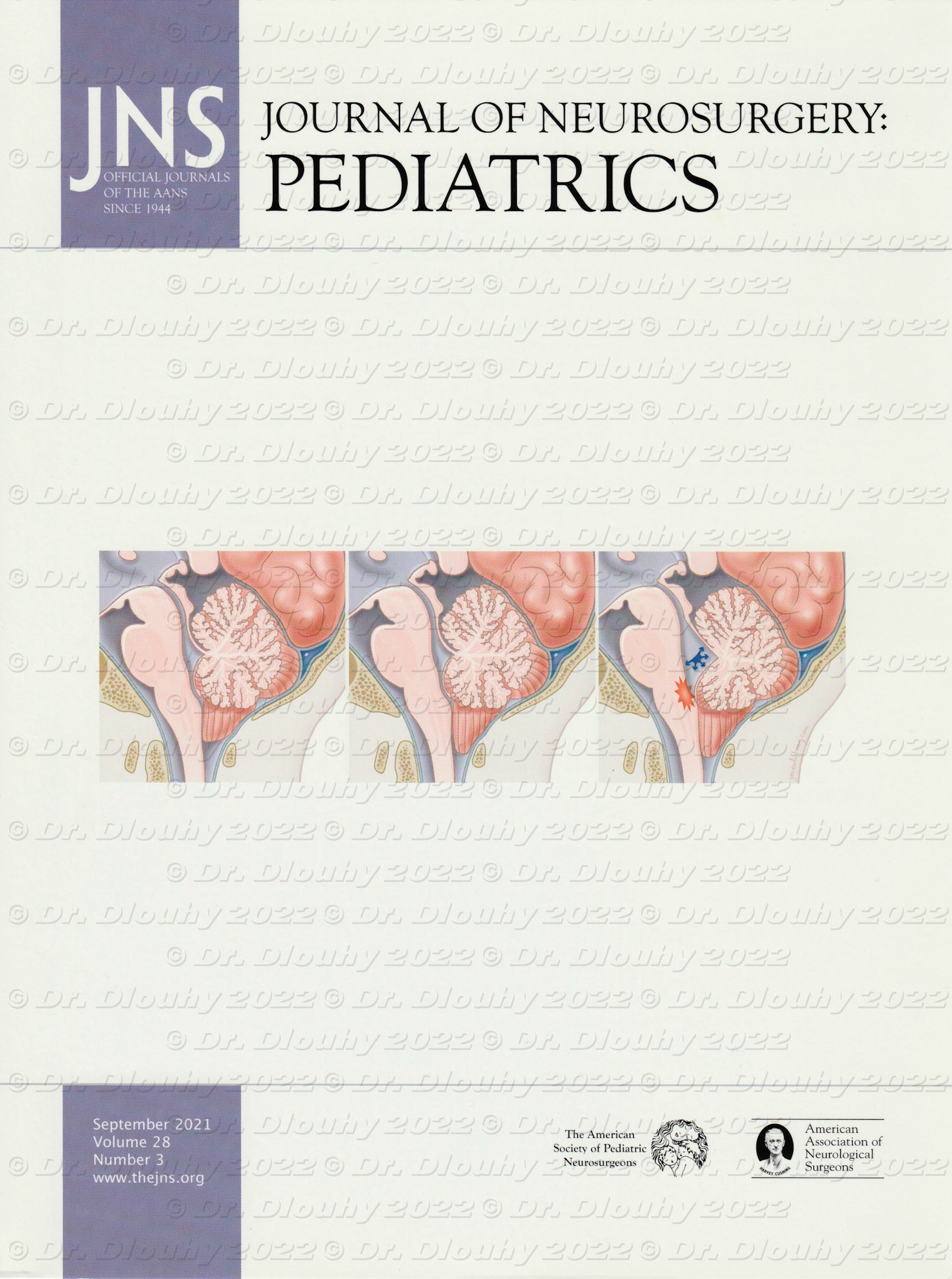
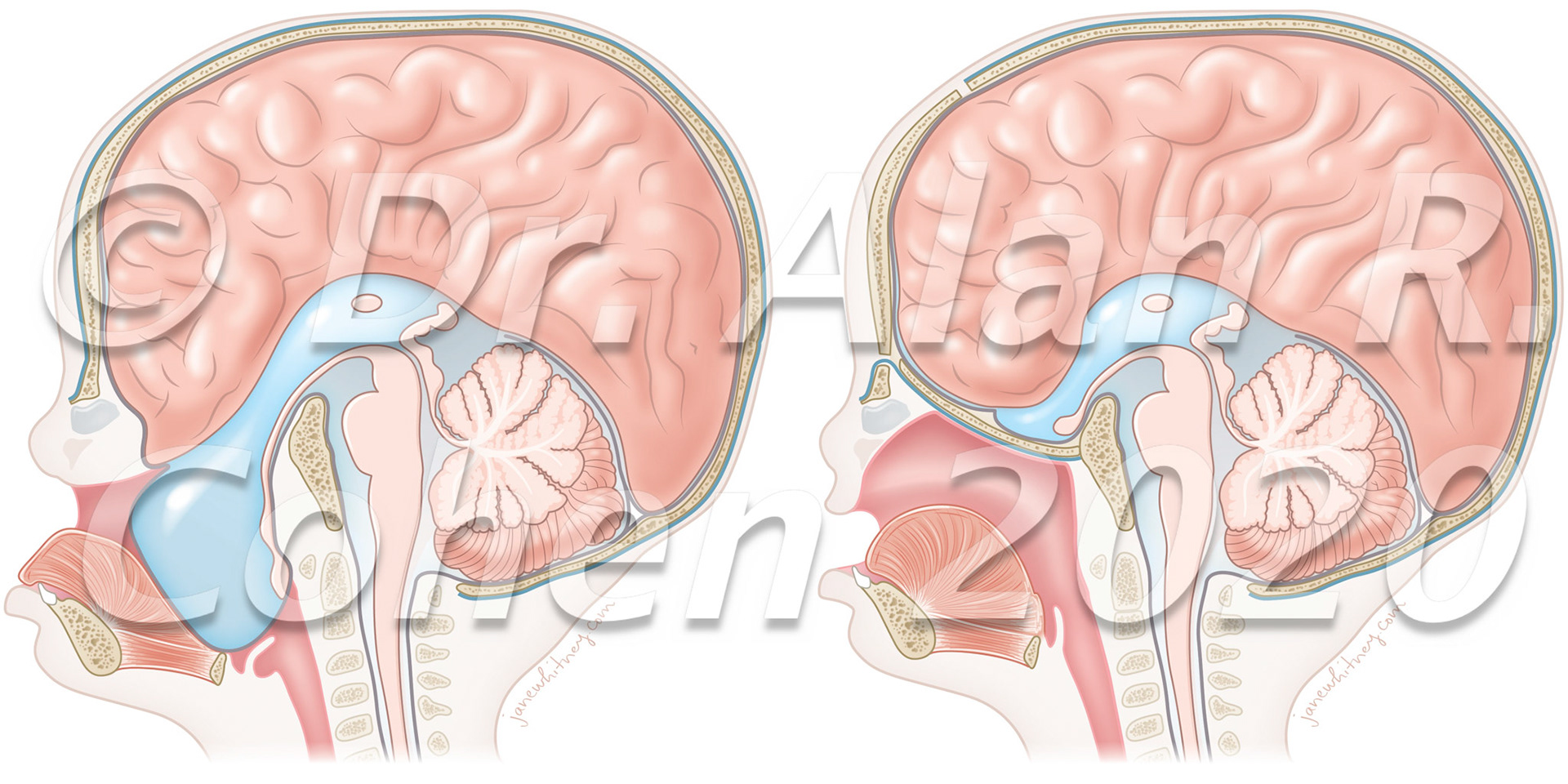
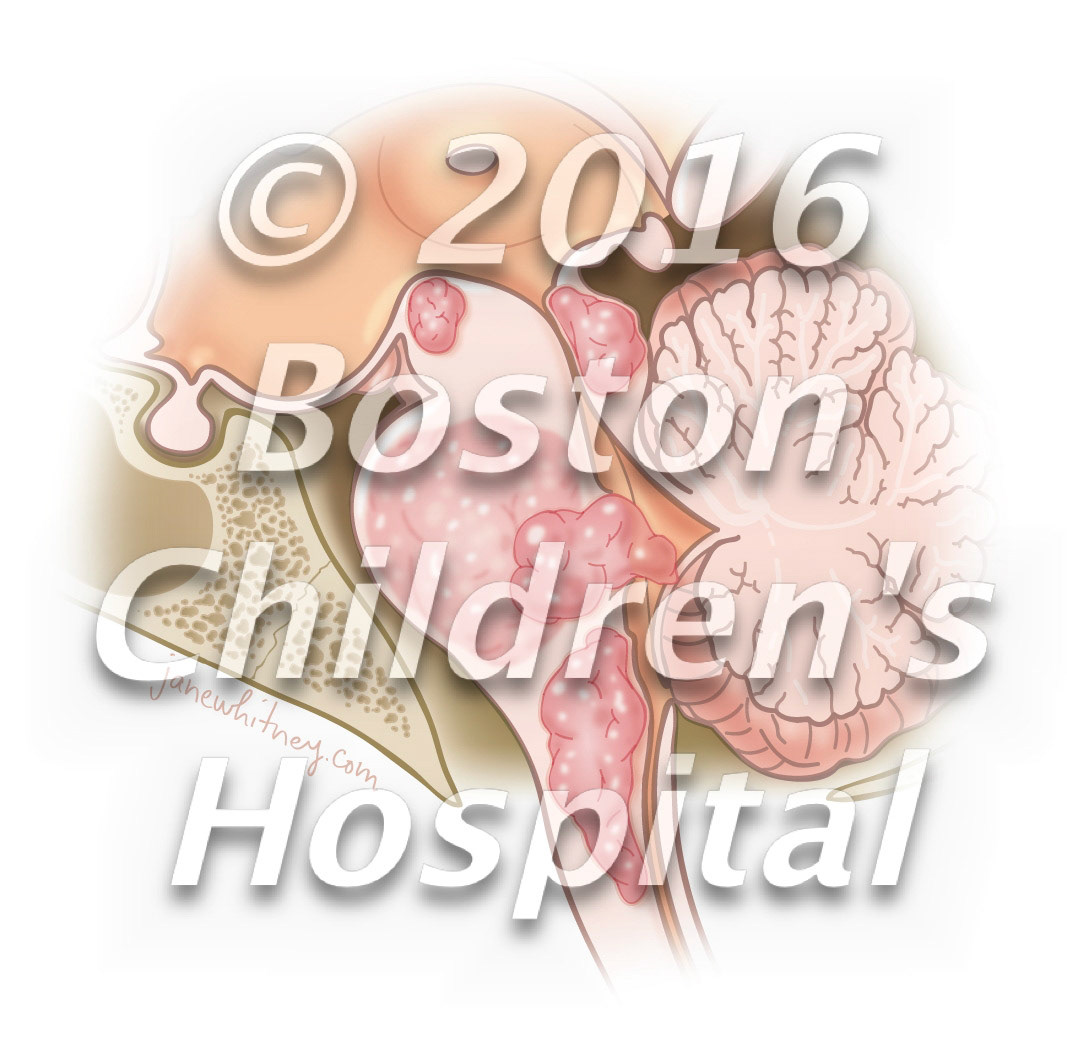
Chiari malformation

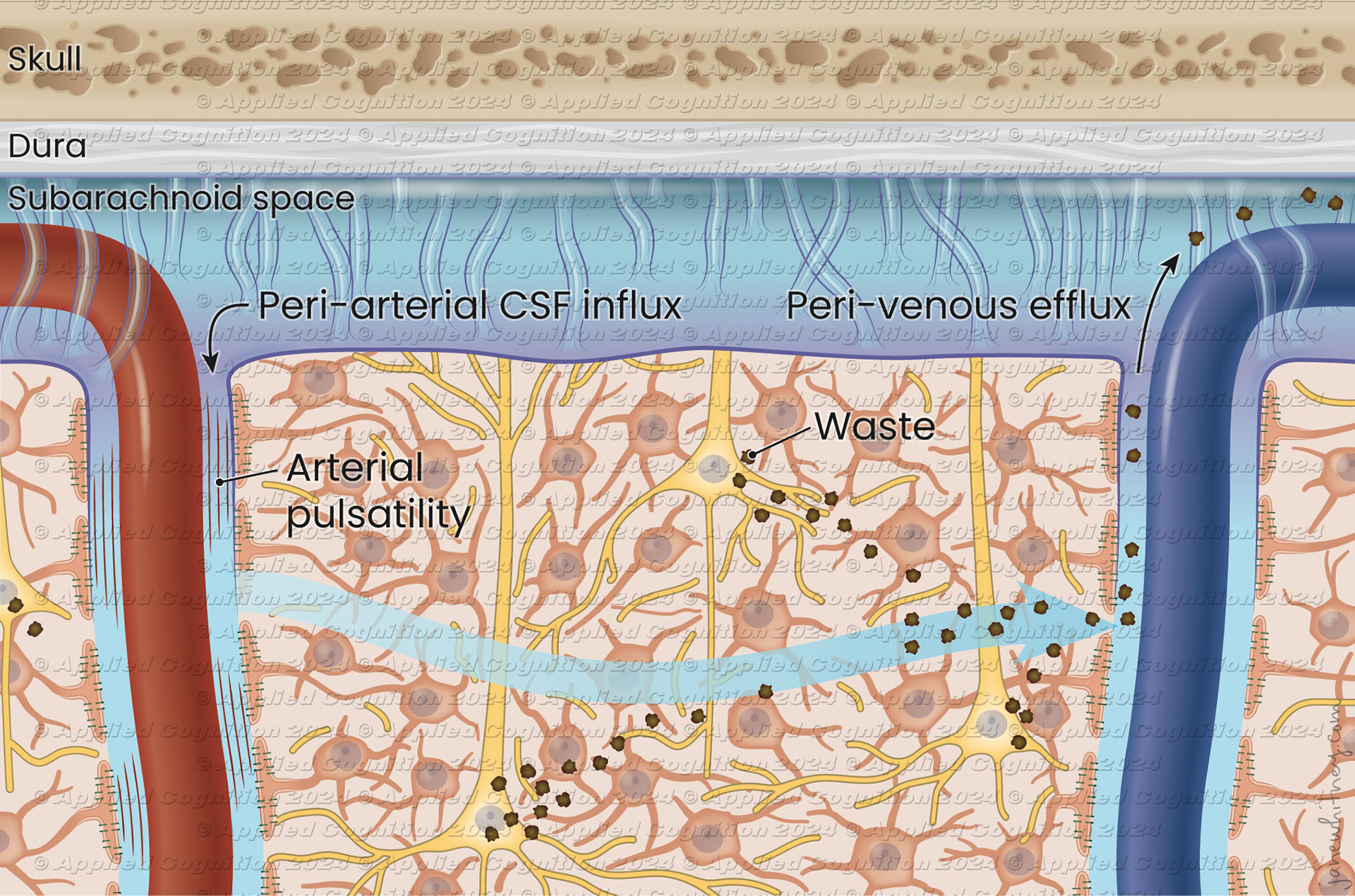
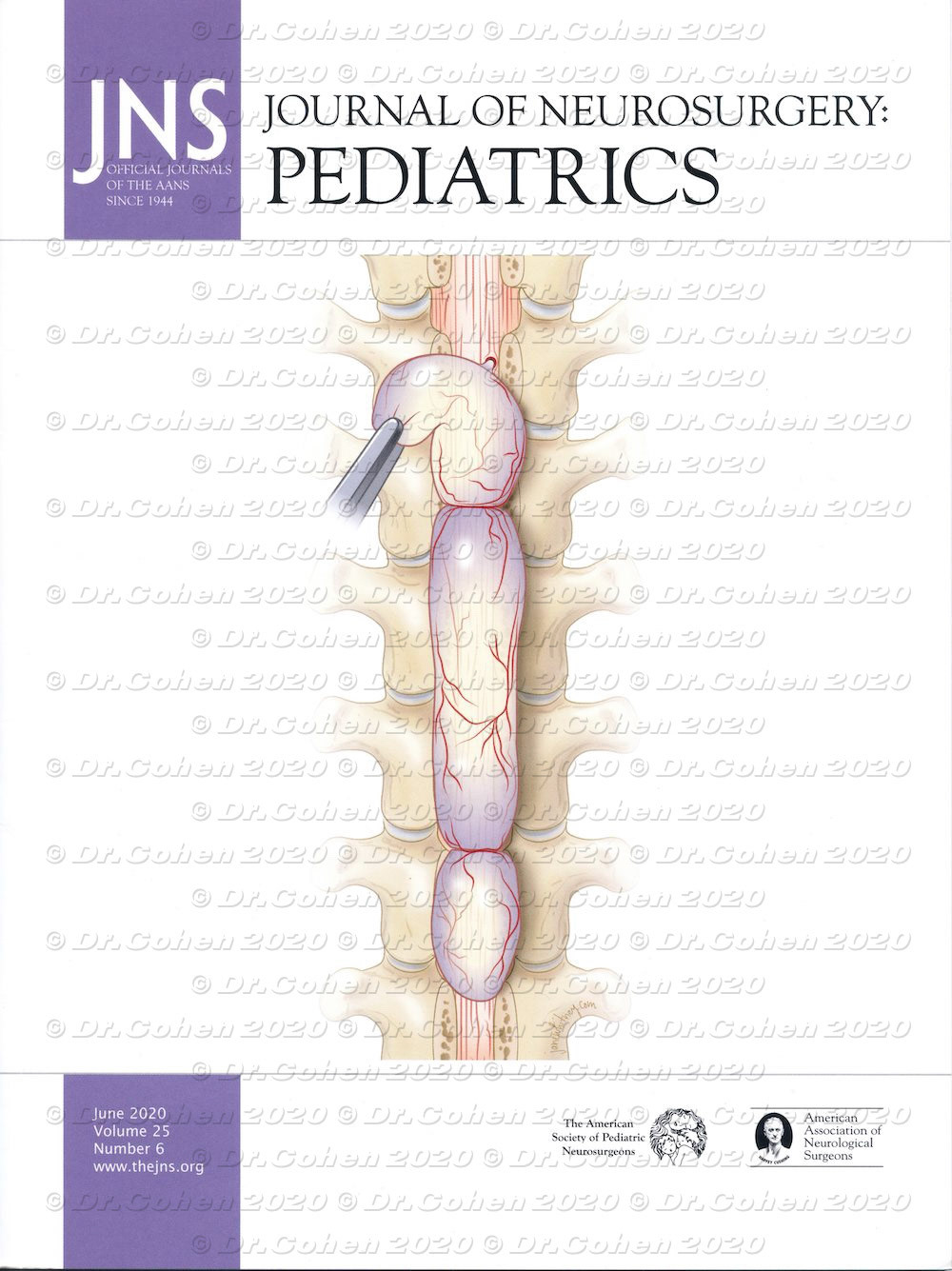
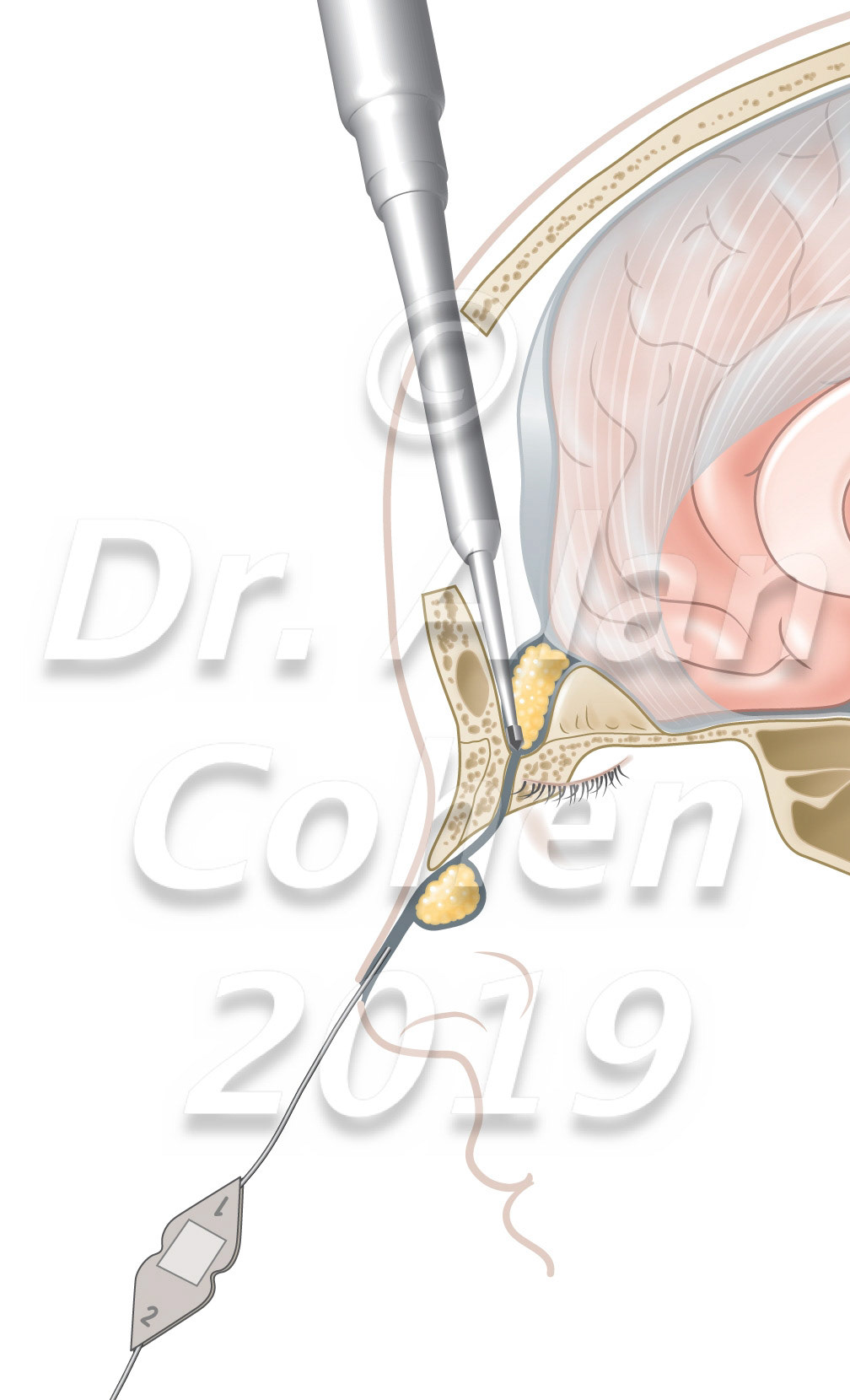
Spinal extradural arachnoid cysts (SEACs) are uncommon spinal lesions that may cause myelopathy, most frequently in the 2nd decade of life. Three contiguous but separate spinal cysts were identified intraoperatively, and they were completely excised with closure of the dural defects. The patient recovered motor and sensory function of the lower extremities. Journal of Neurosurgery: Pediatrics, 2020, cover https://doi.org/10.3171/2019.12.PEDS19108

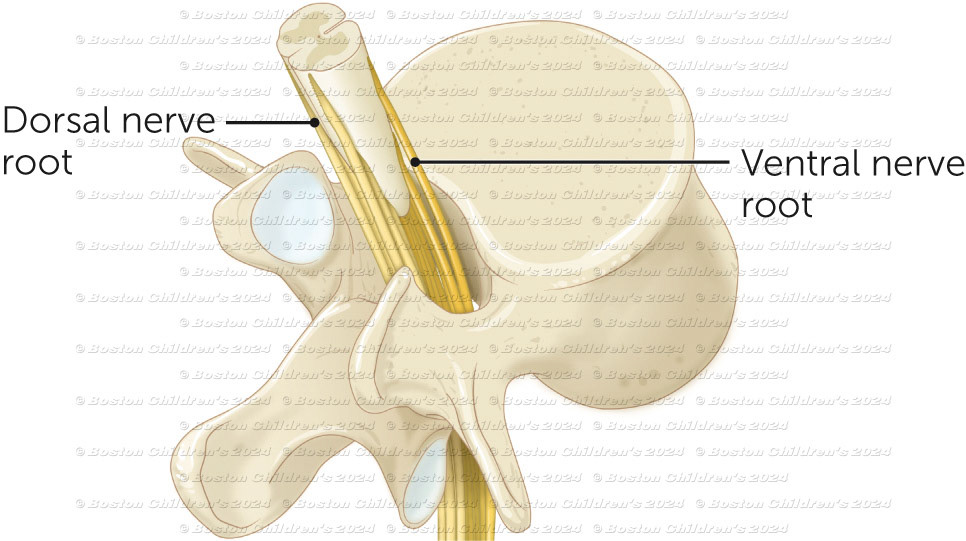
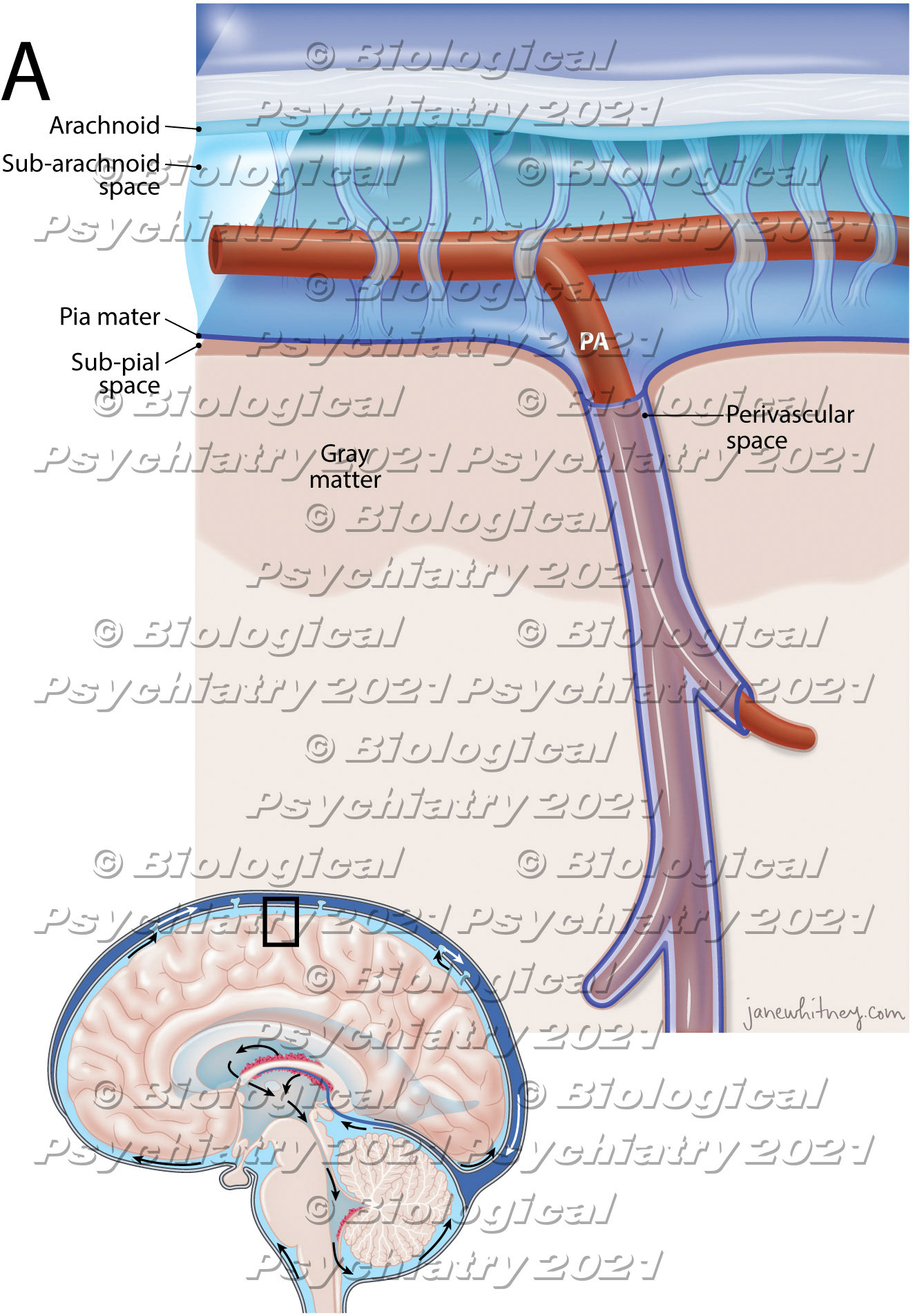
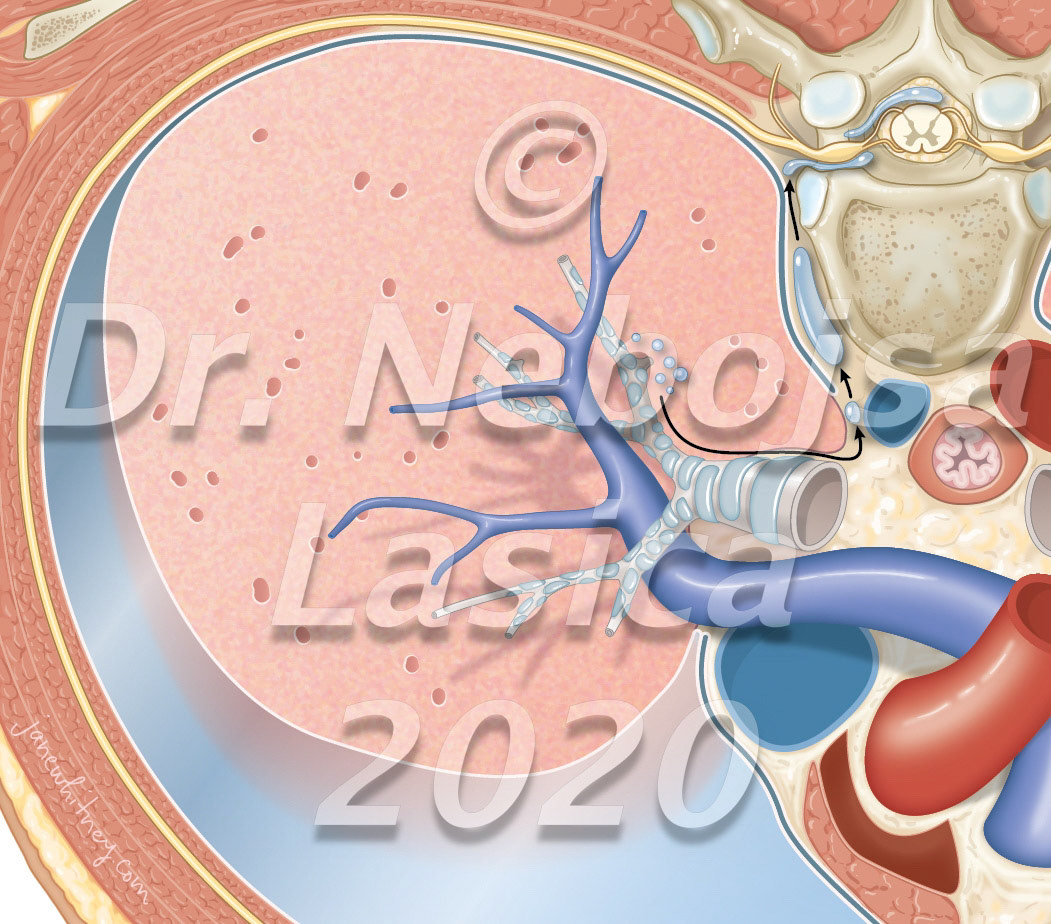
Perivascular spaces, also known as Virchow-Robin spaces are fluid-filled spaces in the brain that surrounds small arterioles, capillaries and venules in the brain.Biological Psychiatry https://doi.org/10.1016/j.biopsych.2021.06.025

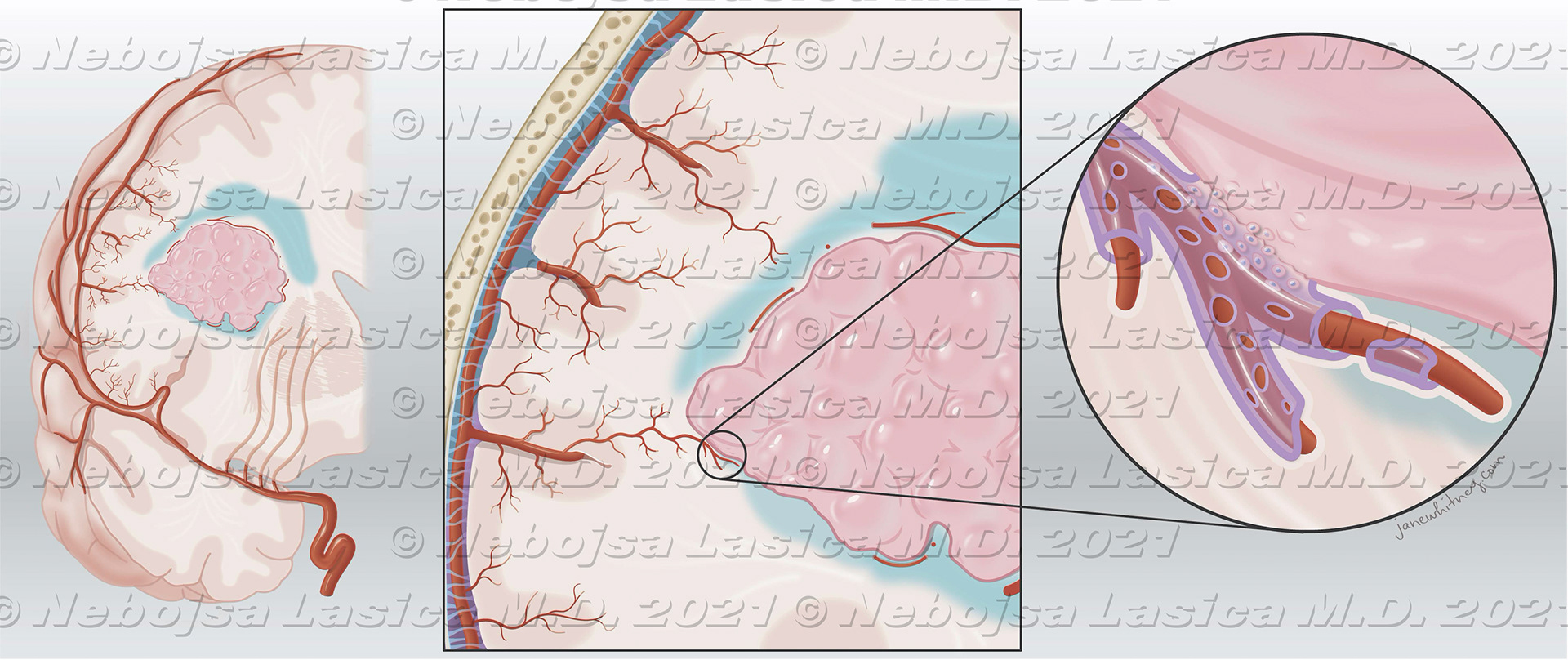
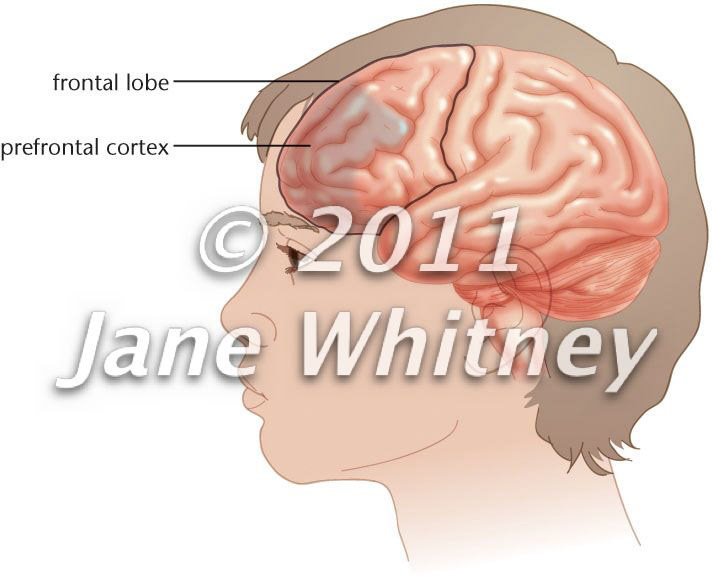
The primary intraparenchymal meningioma of thefrontal lobe (A) with no apparent dural attachment. Thepresumption is that arachnoid cells present in the pia matermigrate together with penetrating blood vessels duringbrain development (B).World Neurosurgery, Sept. 2021https://doi.org/10.1016/j.wneu.2021.06.139

Before (left) and after (right) of a large encephalocele (herniation of meninges and brain) through the base of the anterior skull into the mouth.

Pneumorrhachis: The most frequent initial mechanism is an increase in intraalveolar pressure (acute asthma, recurrent vomiting, or closed thoracic trauma). Barotrauma and alveolar rupture allow air migration along the bronchial tree up to the mediastinum. The collected air then separates the mediastinal pleura from the aorta and the parietal pleura from the spine; therefore, it enters the epidural space via the intervertebral foramina. The suddenness, more than the size of the pneumothorax, induces this initial increase in intra-alveolar pressure. Journal of Neurosurgery: Spine Oct 2020 https://doi.org/10.3171/2020.6.SPINE20648

Meet in the middle technique. The neurosurgeon removes the intracranial cyst and sinus tract working through a small bifrontal craniotomy and drilling through the foramen cecum. The plastic surgeon excises the nasal punctum and uses an external rhinoplasty to remove the extracranial lesion. Child's Nervous System, 2020 https://doi.org/10.1007/s00381-020-04499-5

Tube within tube

Tentorium

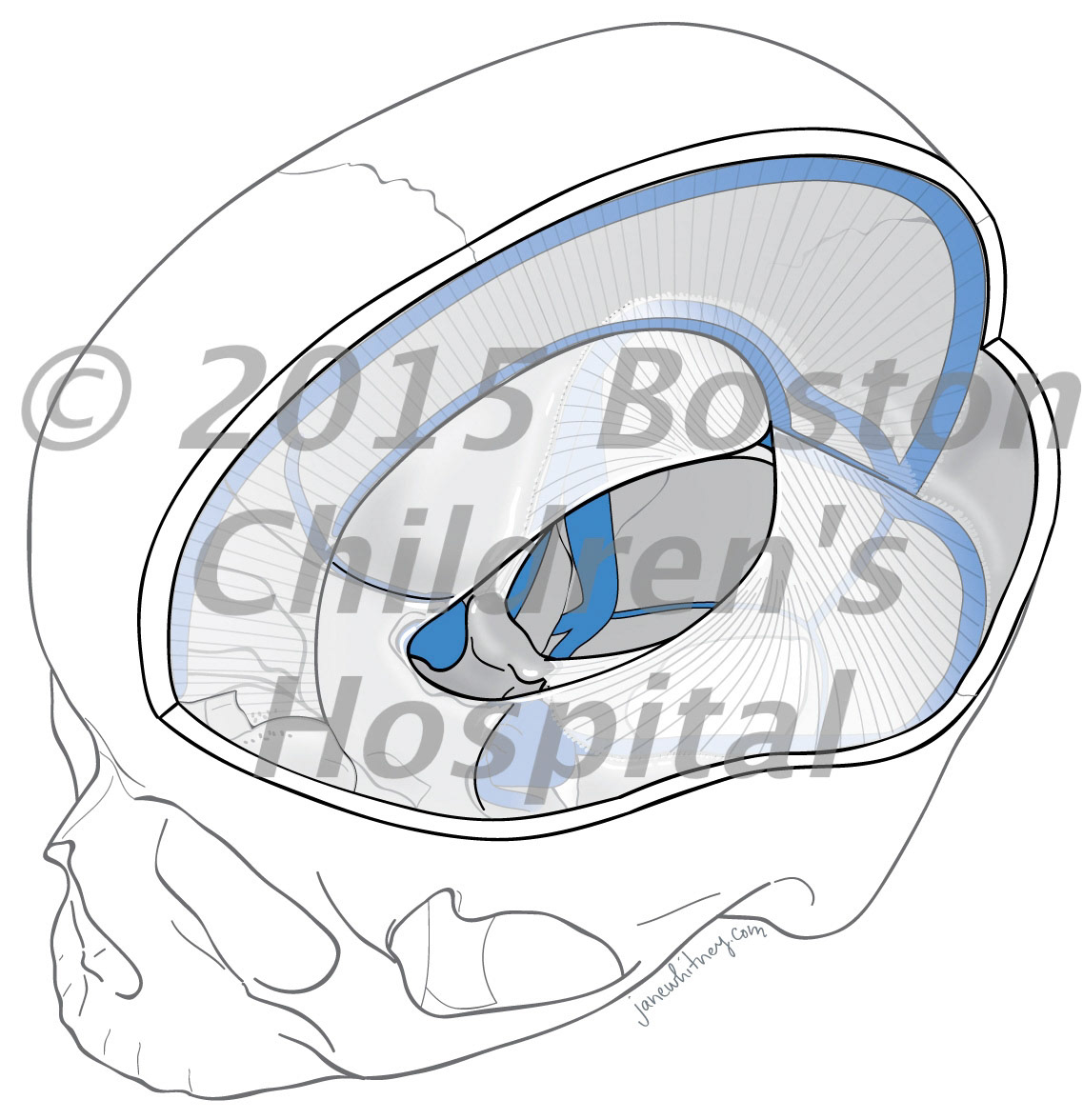
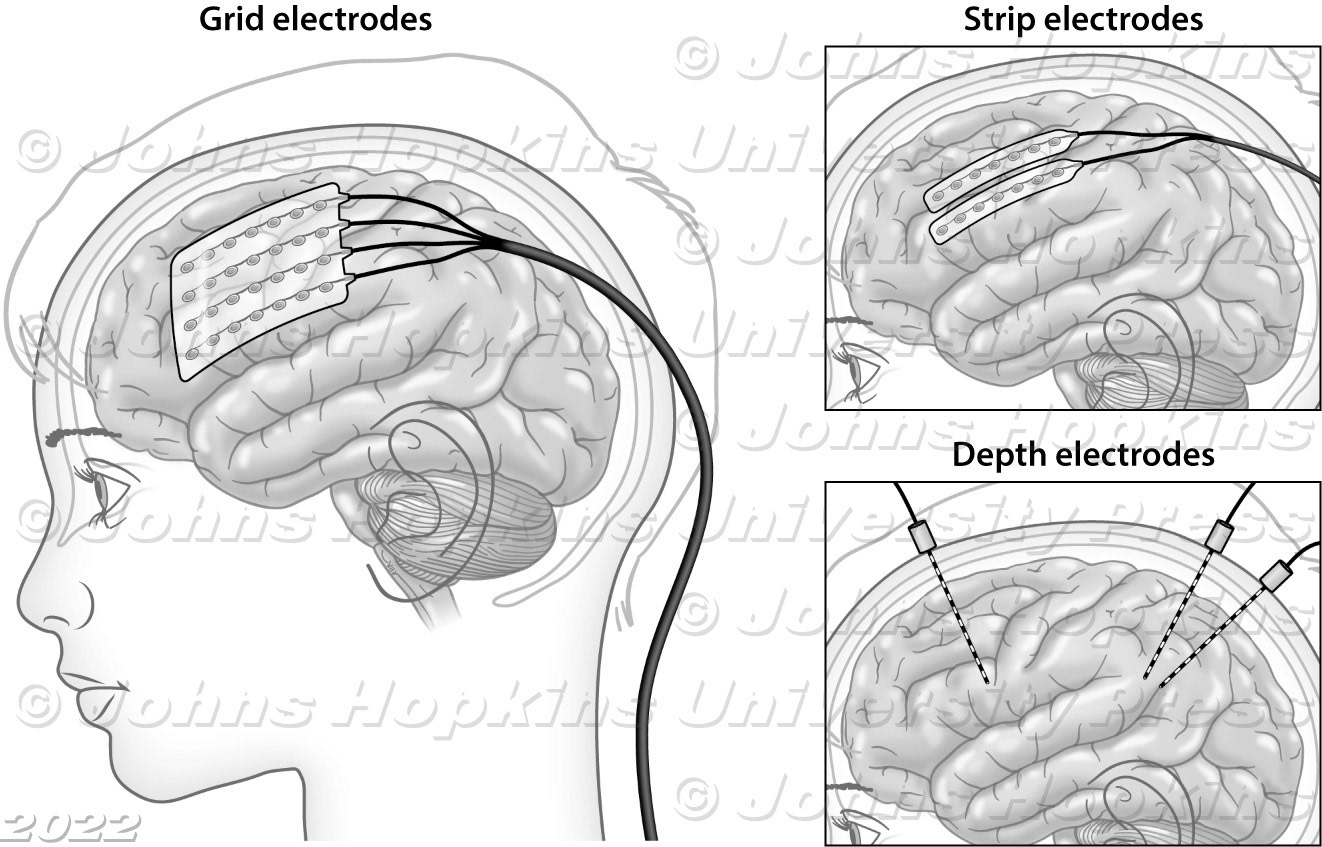
Invasive EEG monitoring for epilepsy

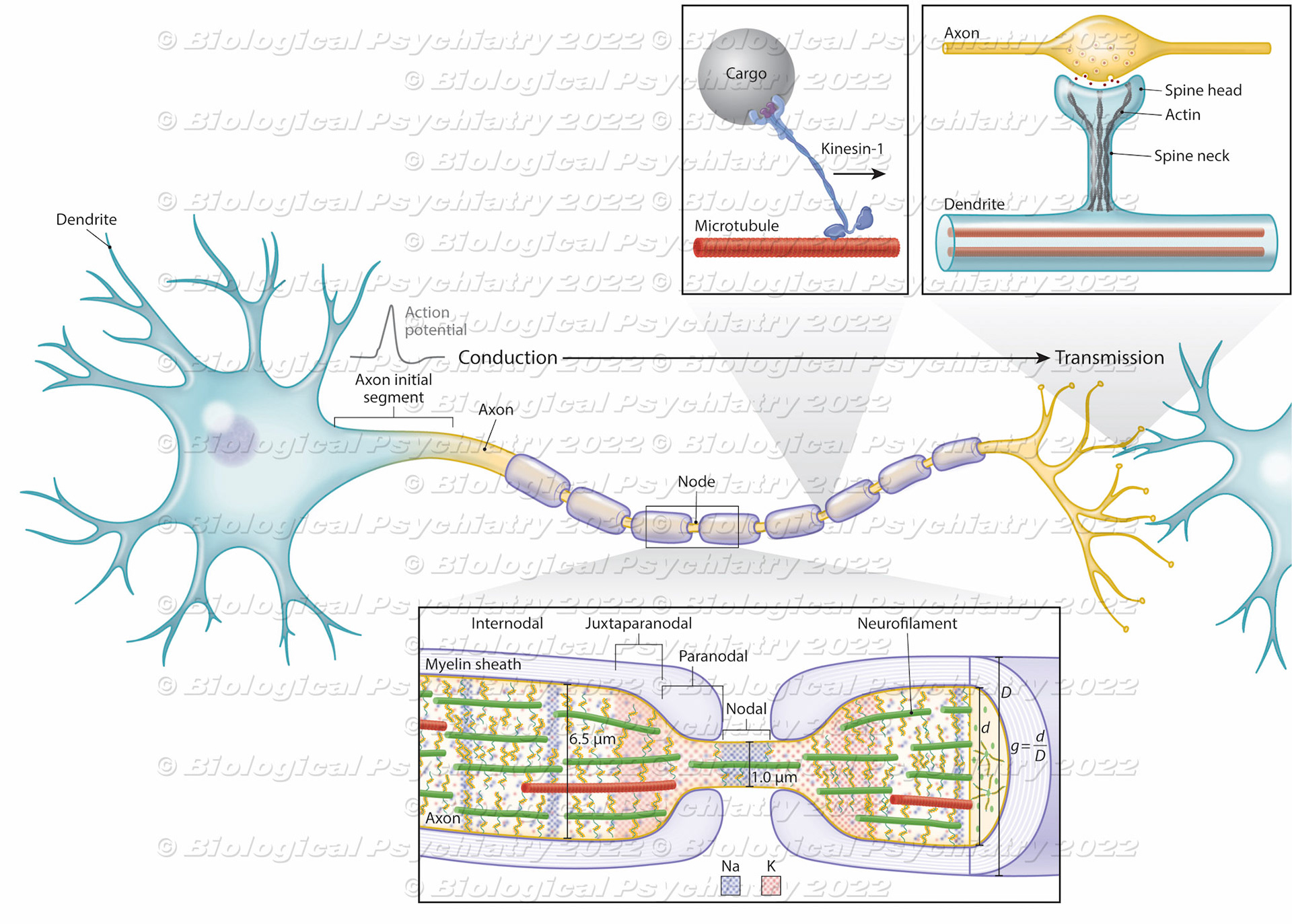
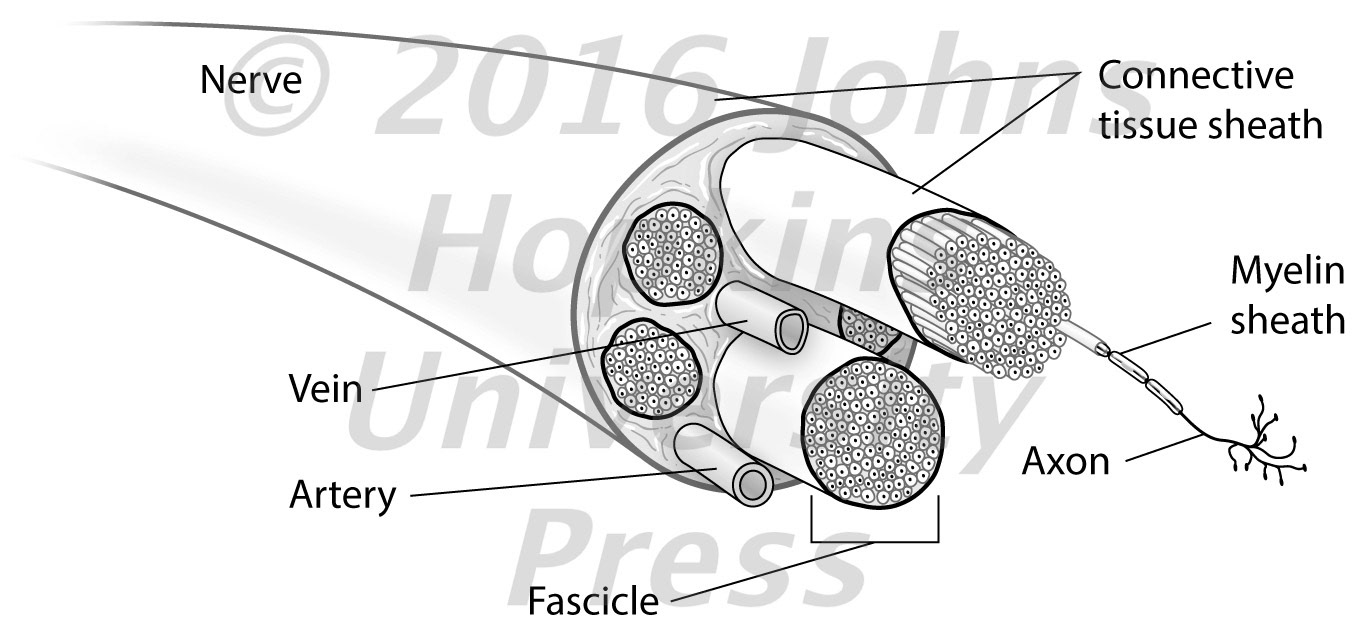
Nerve conduction and transmission: Key cellular components

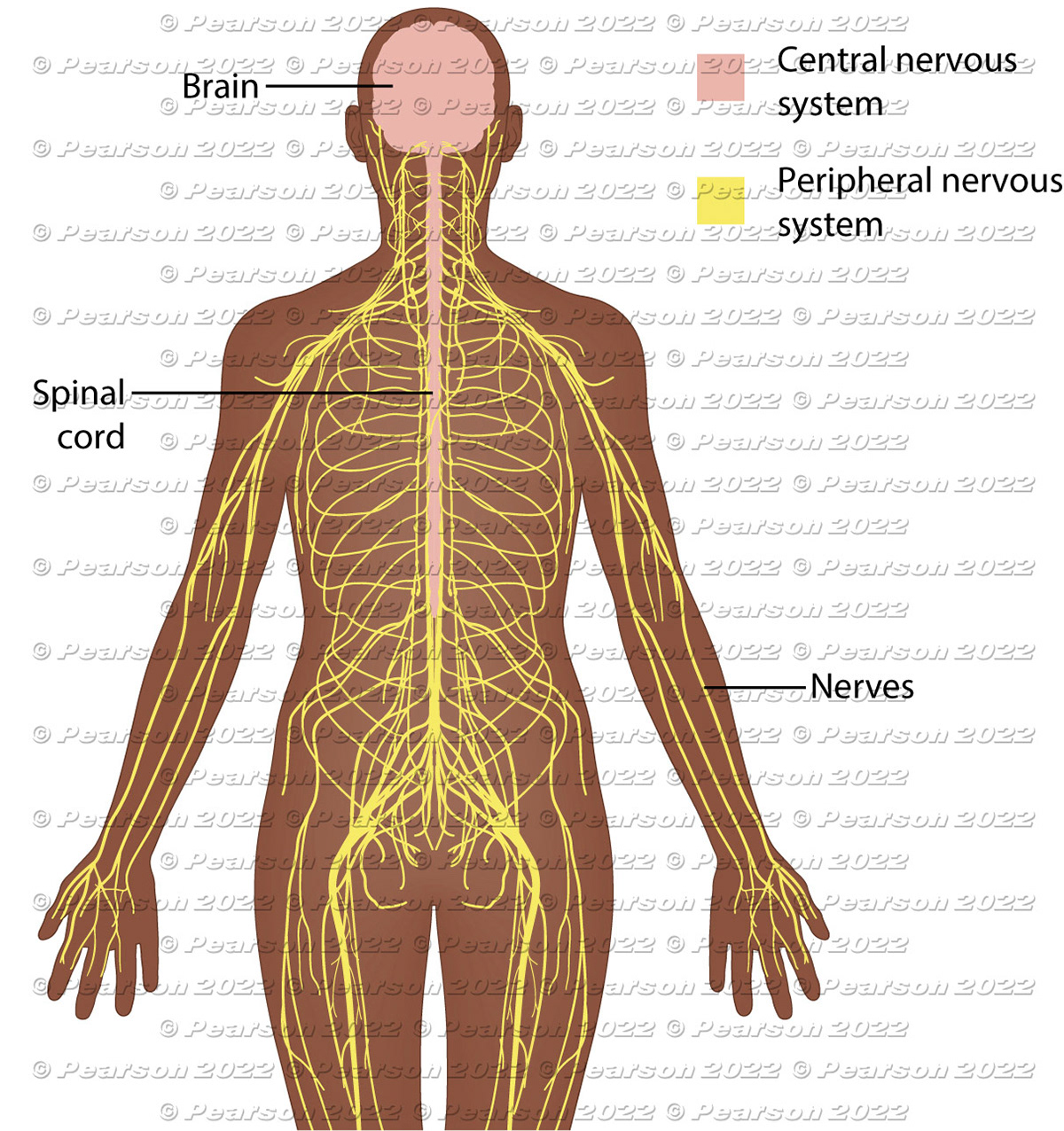
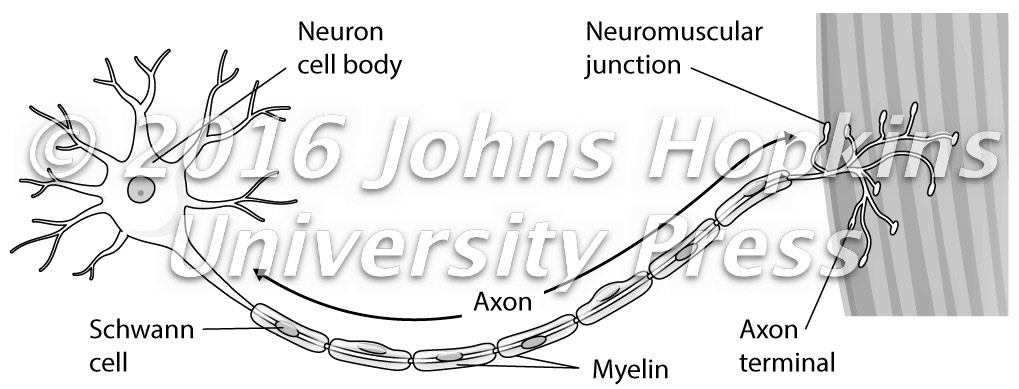
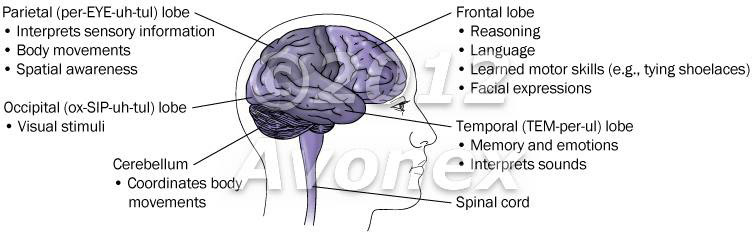
Human nervous system

ER 2018-00017_Fig 1+k+j2

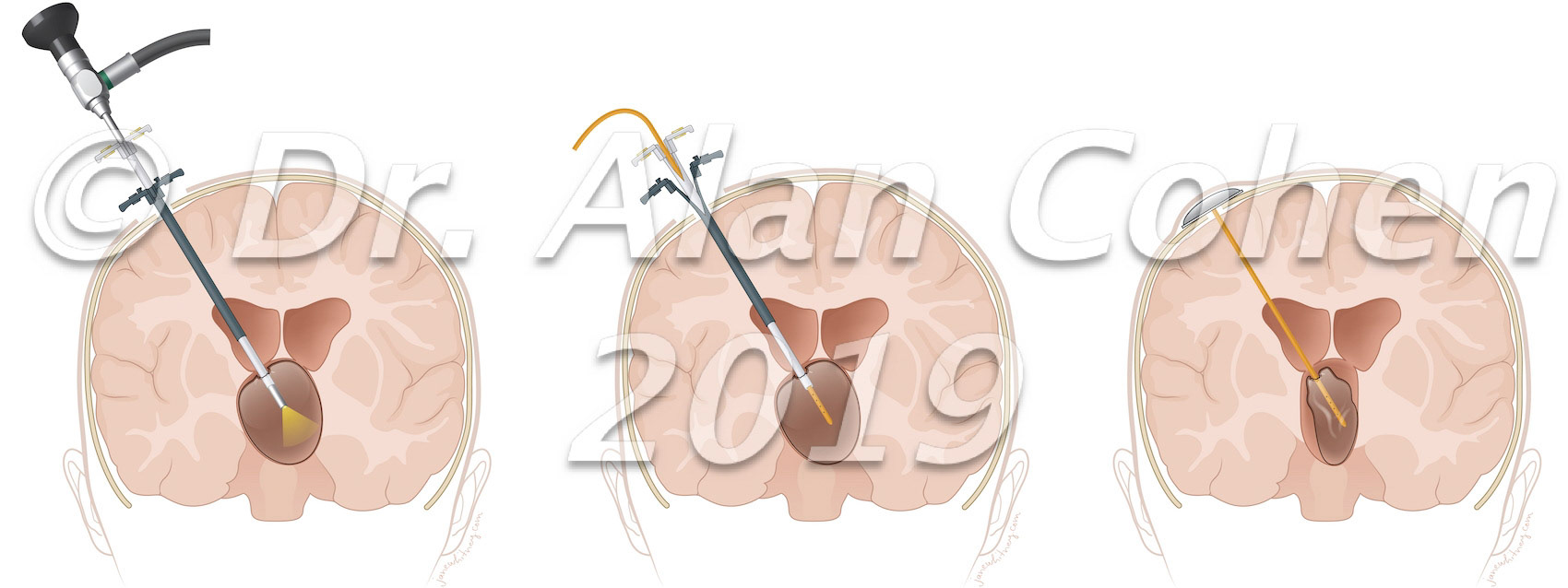
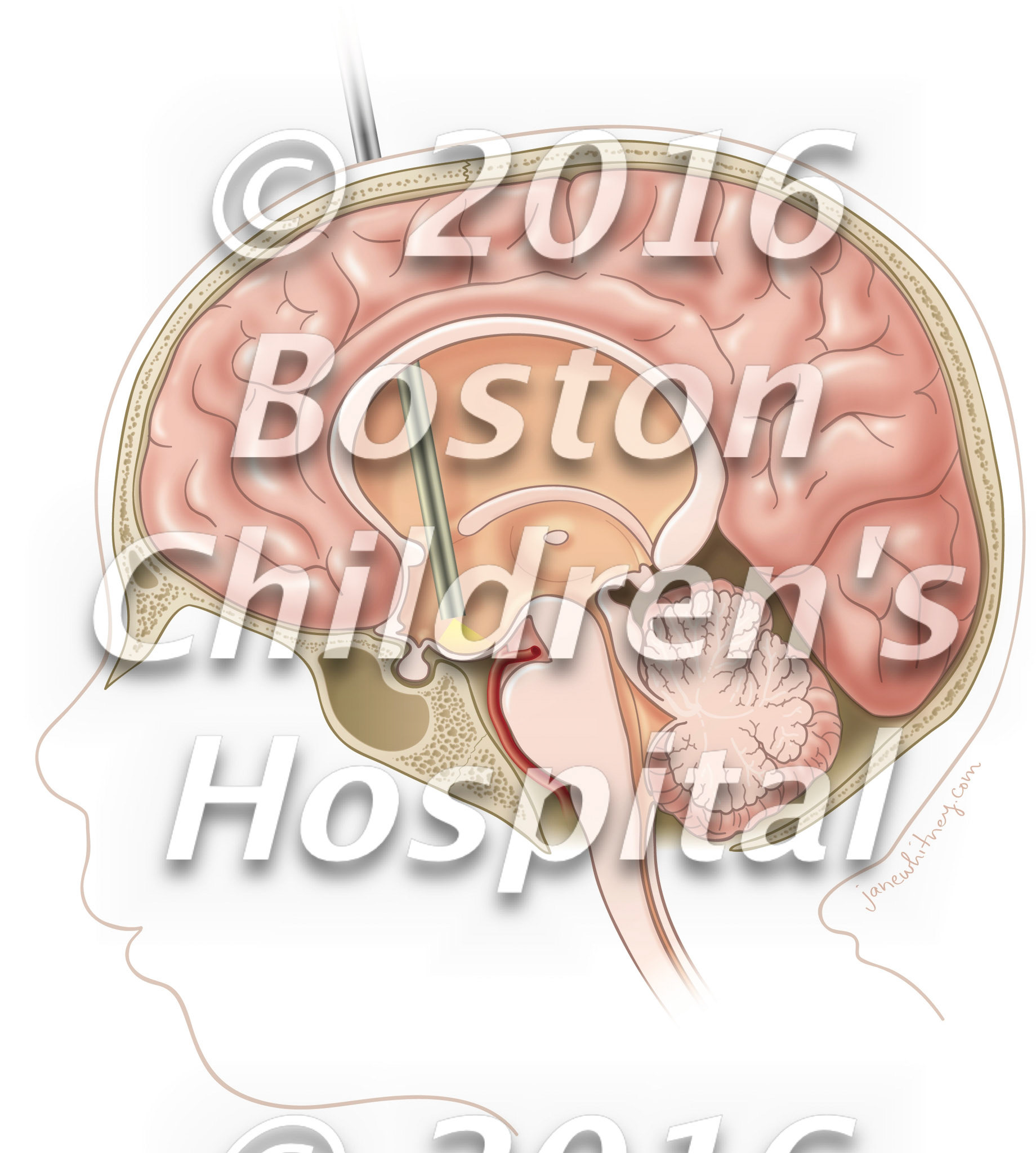
Figure_1_ETV_draft9

Brainstem_Gliomas_final

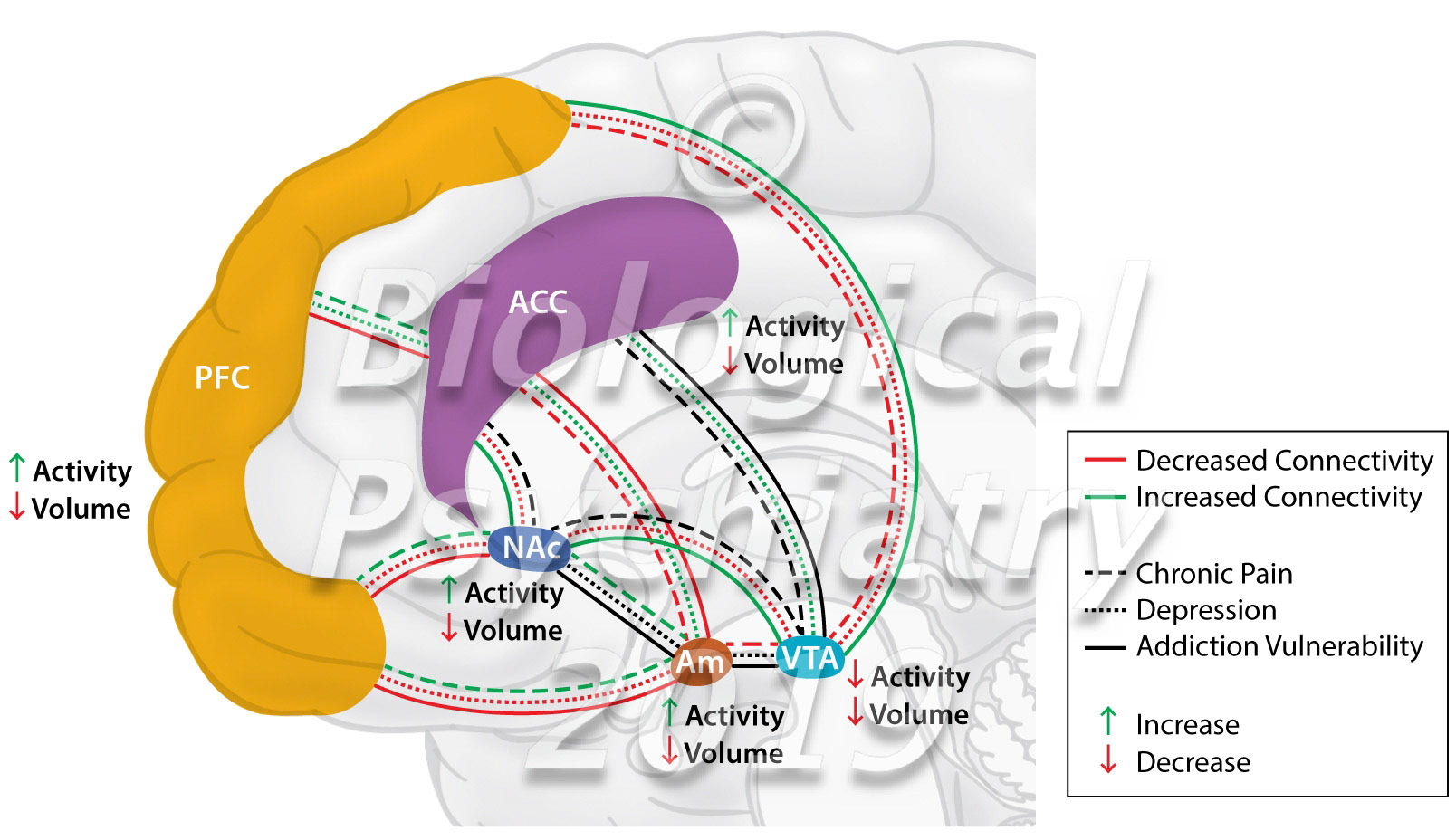
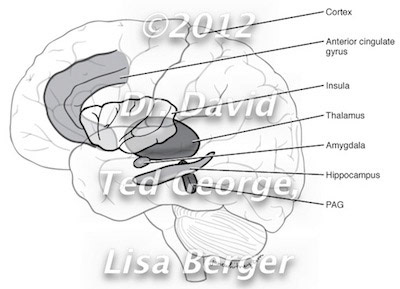
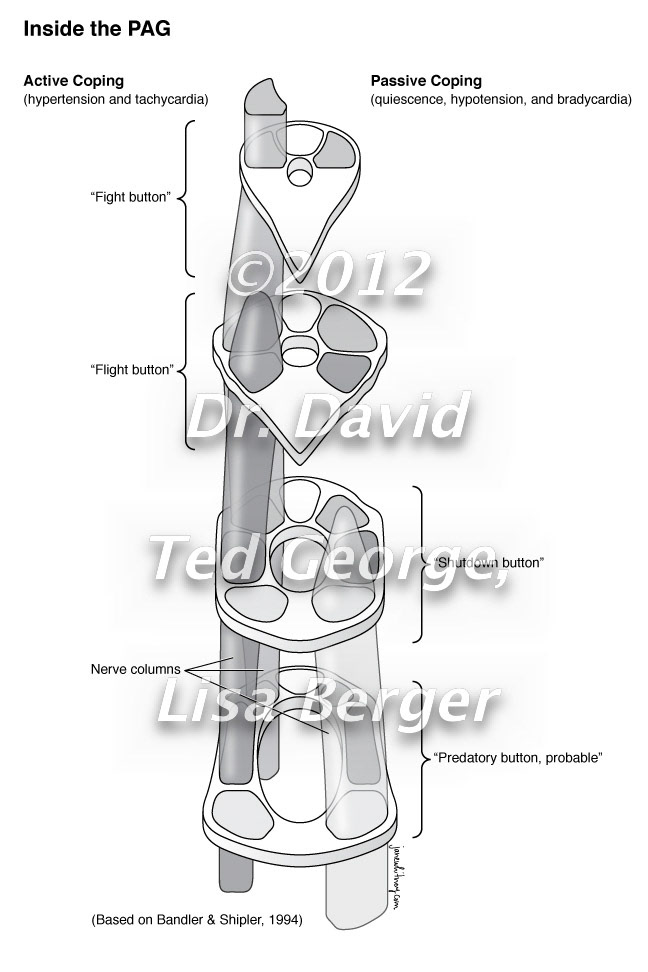
The Mesolimbic Dopamine System in Chronic Pain and Associated Affective Comorbidities Biological Psychiatry https://doi.org/10.1016/j.biopsych.2019.10.018

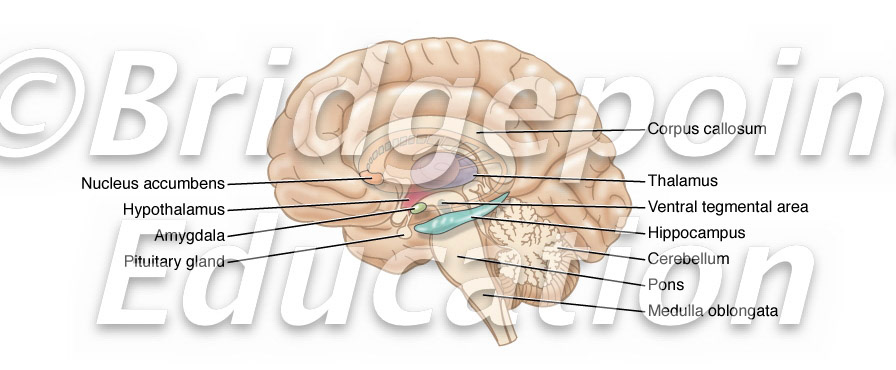
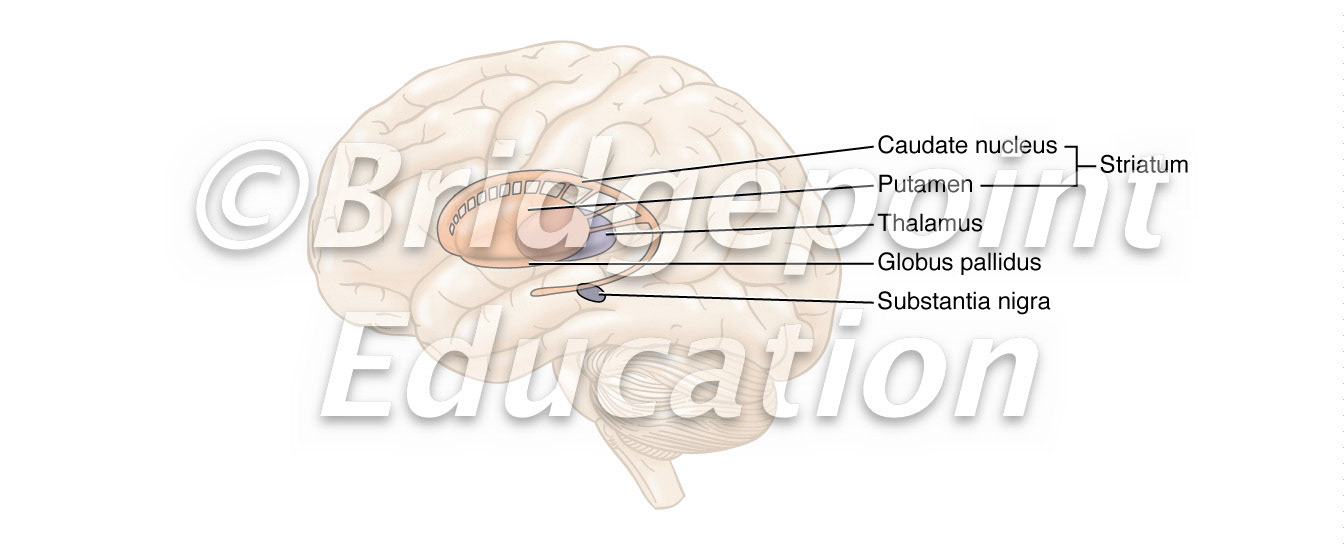
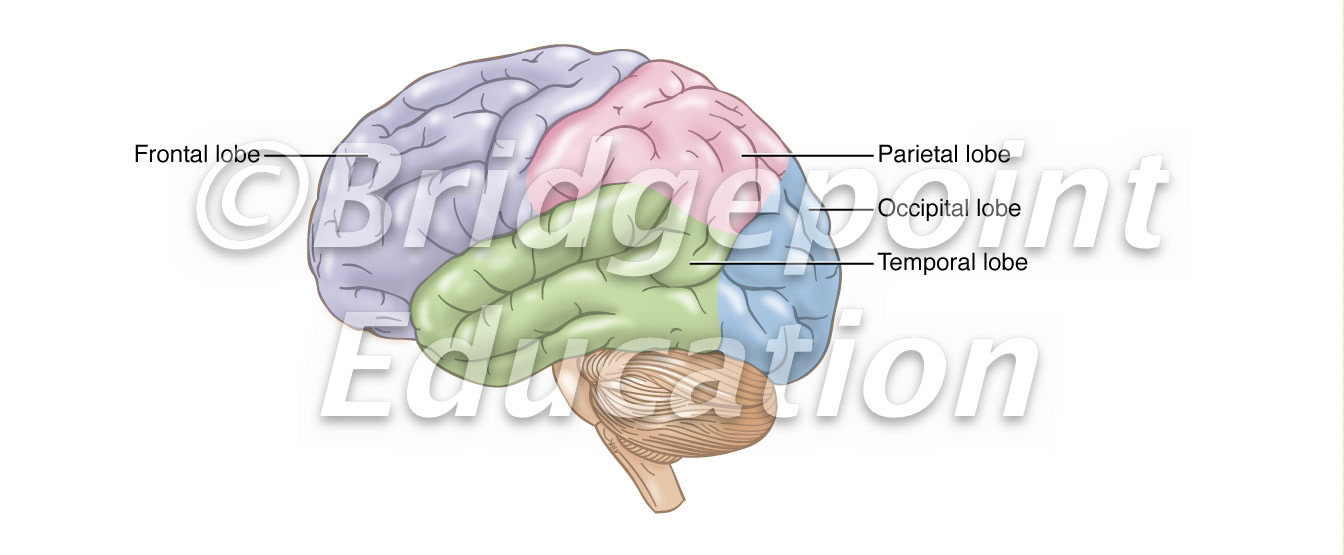
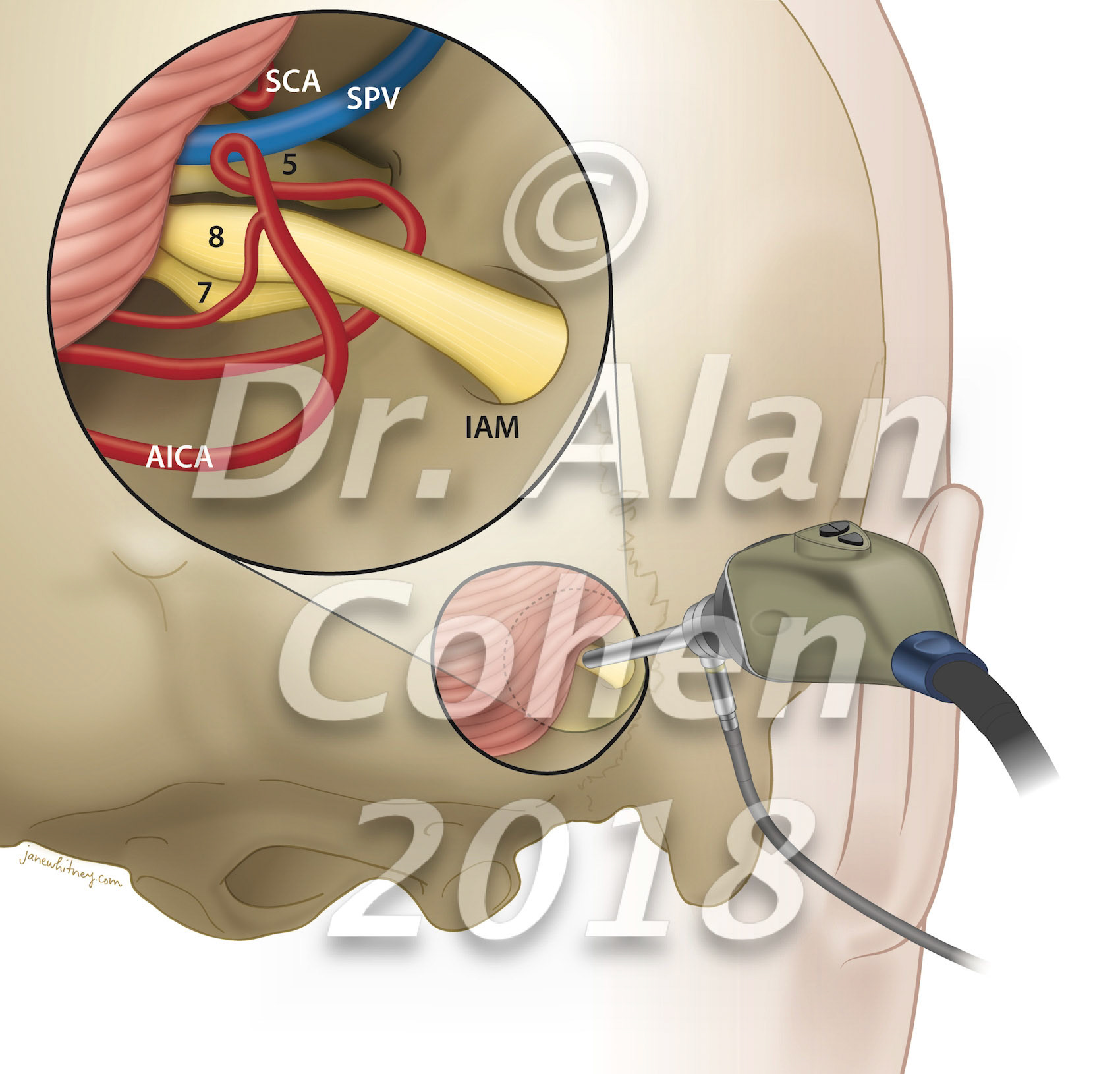
Brain structures involved in psychiatric conditions

Endoscope-assisted microsurgery of the posterior fossa. Cerebellum is retracted; retractor not shown. SCA: superior cerebellar artery. SPV: superior petrosal vein. AICA: anterior inferior cerebellar artery. IAM: internal acoustic meatus.

Nerve structure

Neuron, neuromuscular junction

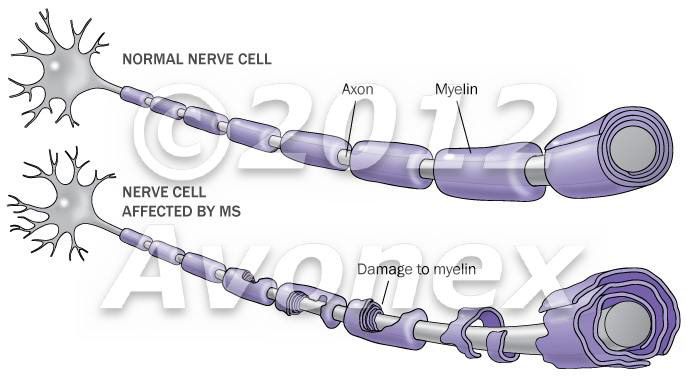
Multiple sclerosis

JANE FASE7-Theme3rough3

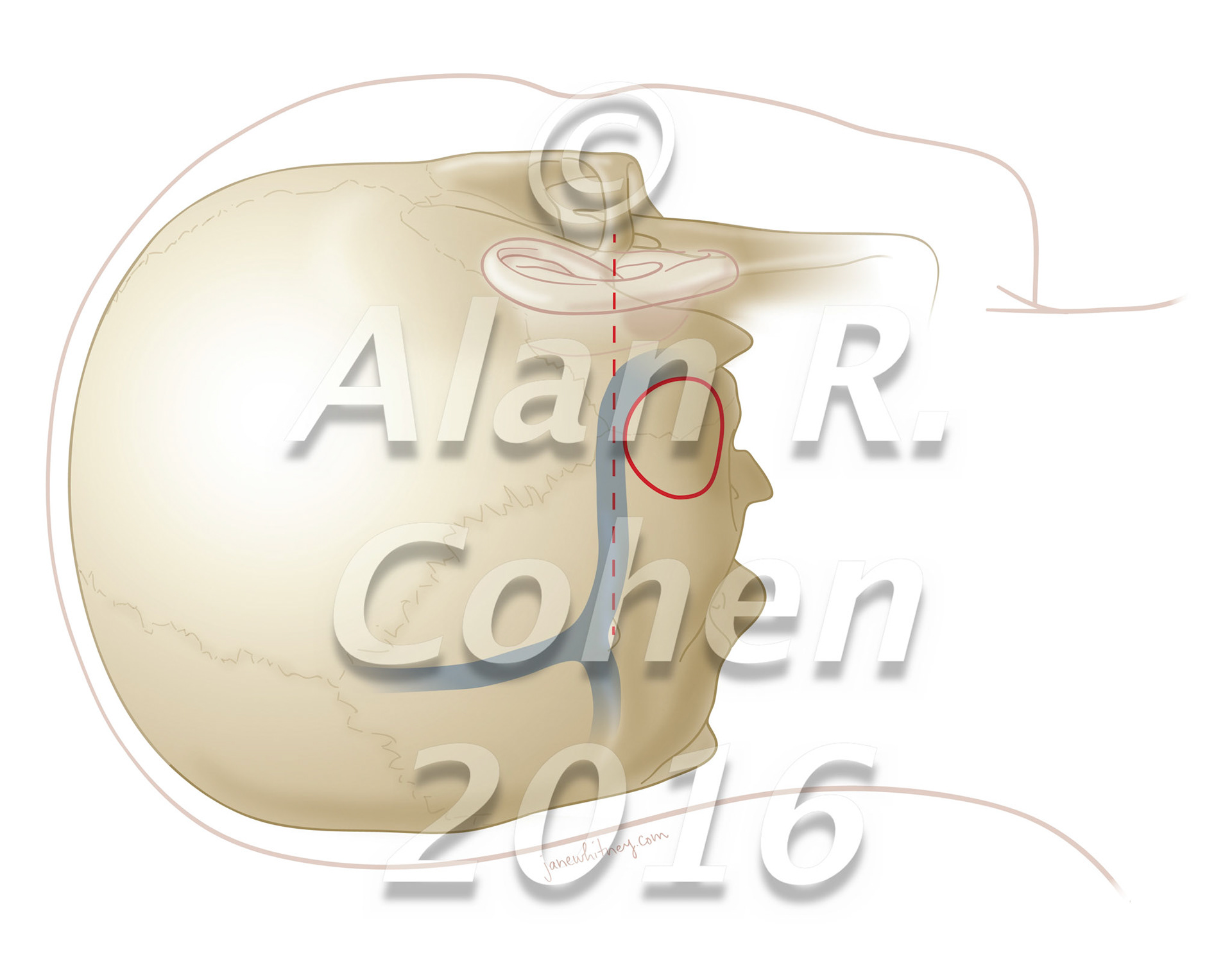
Despite recent technological advances, direct approaches to the posterolateral incisural space remain surgical challenges. The extreme lateral infratentorial supracerebellar approach to treat pathologies located in the ambient cistern and posterior incisural space is a technically feasible route in selected cases. World Neurosurgery, July 2016 https://doi.org/10.1016/j.wneu.2016.04.017

Despite recent technological advances, direct approaches to the posterolateral incisural space remain surgical challenges. The extreme lateral infratentorial supracerebellar approach to treat pathologies located in the ambient cistern and posterior incisural space is a technically feasible route in selected cases. World Neurosurgery, July 2016 https://doi.org/10.1016/j.wneu.2016.04.017

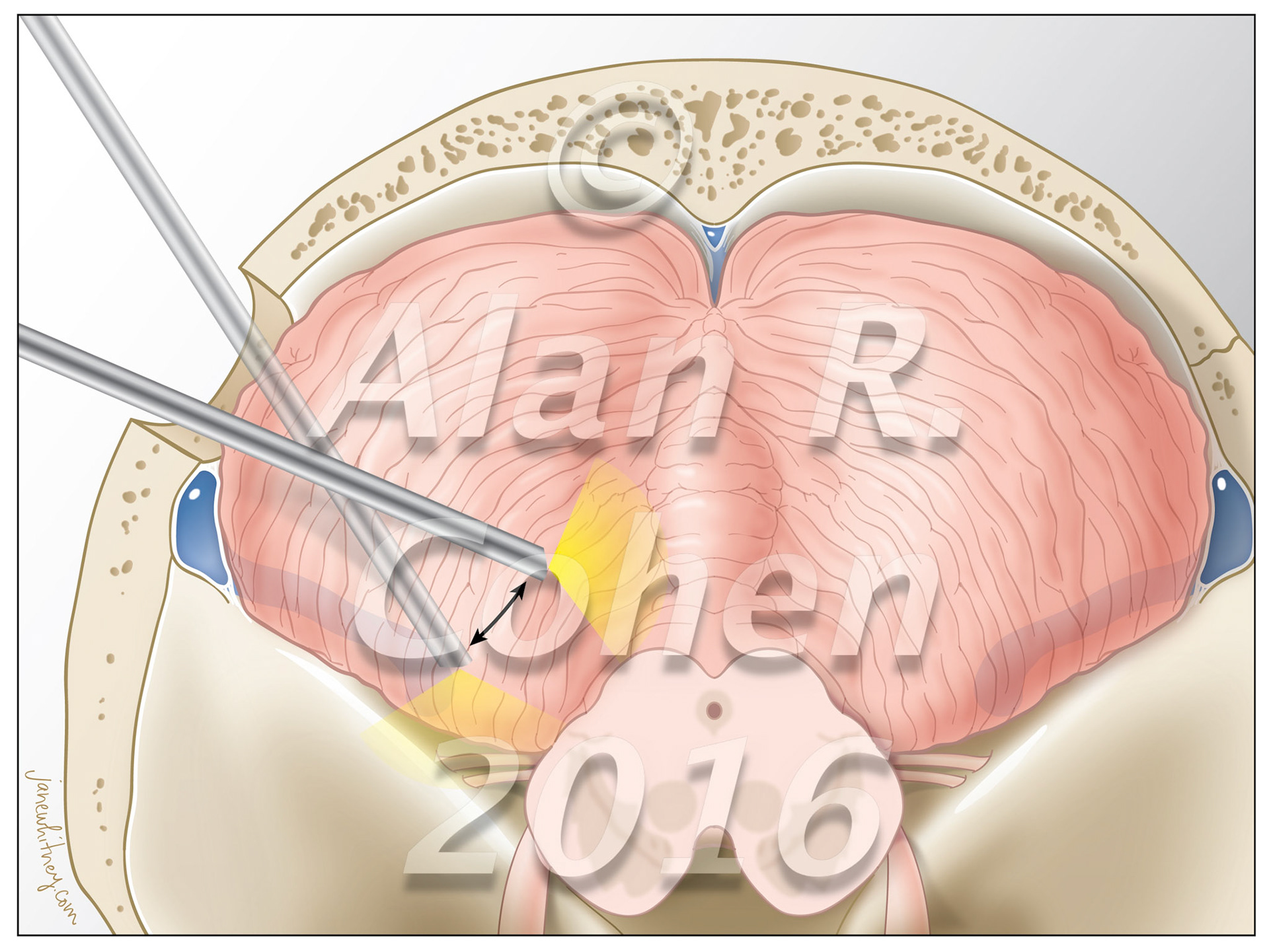
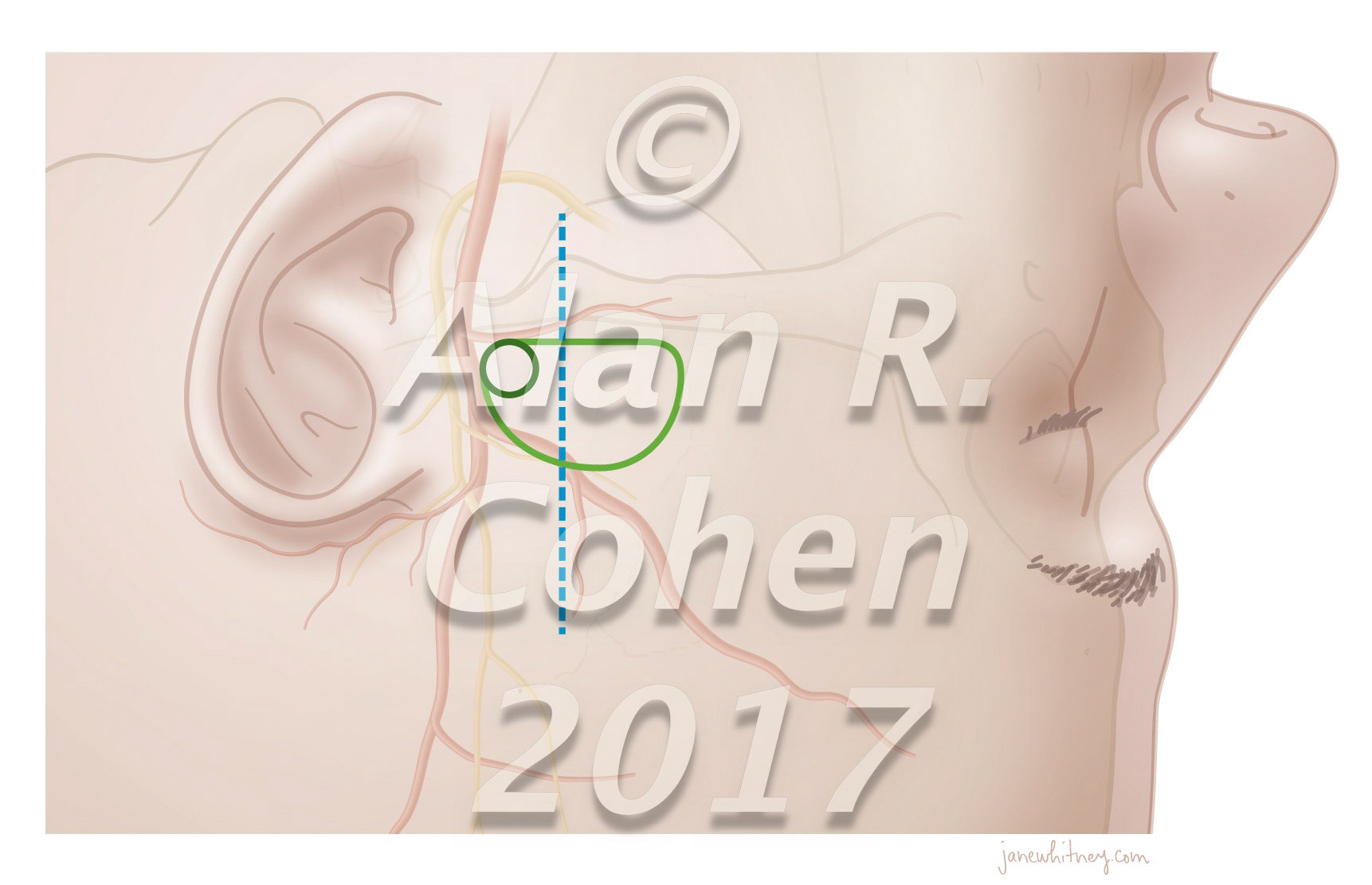
Endoscope-Assisted Microsurgical Subtemporal Keyhole Approach to the Posterolateral Suprasellar Region and Basal Cisterns World Neurosurgery July 2017 https://doi.org/10.1016/j.wneu.2017.02.054

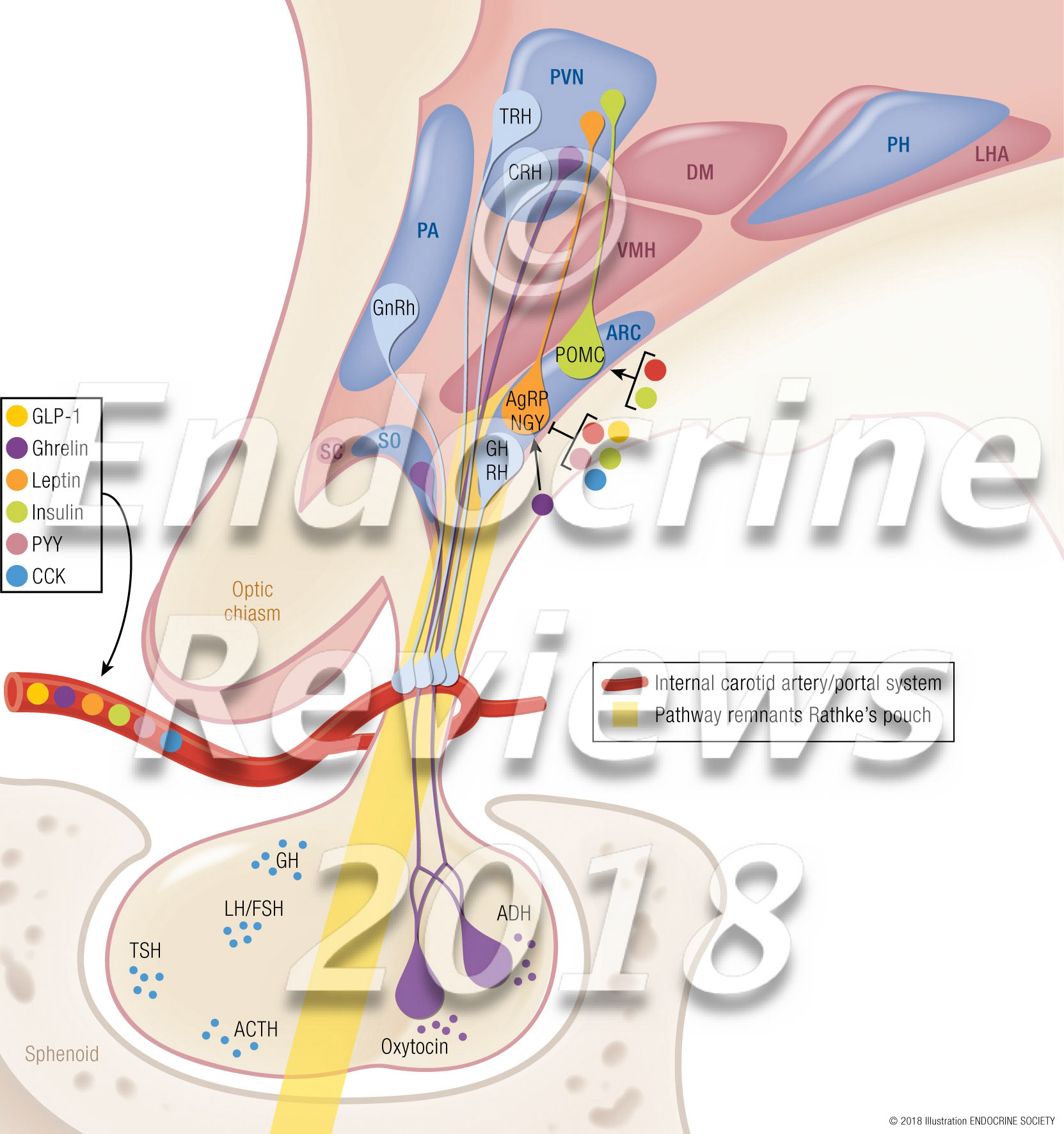
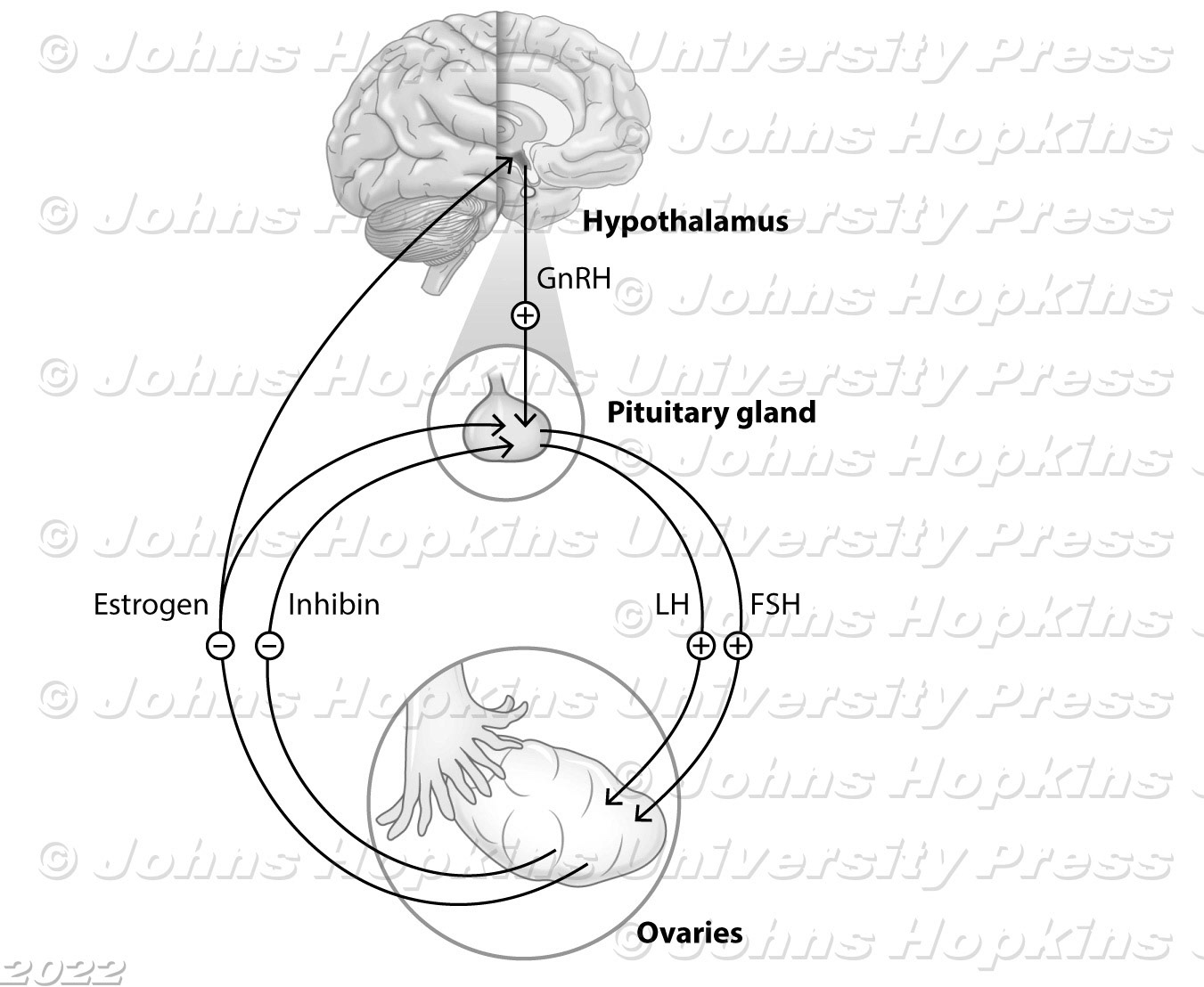
Hypothalamic-Pituitary-Ovarian Axis